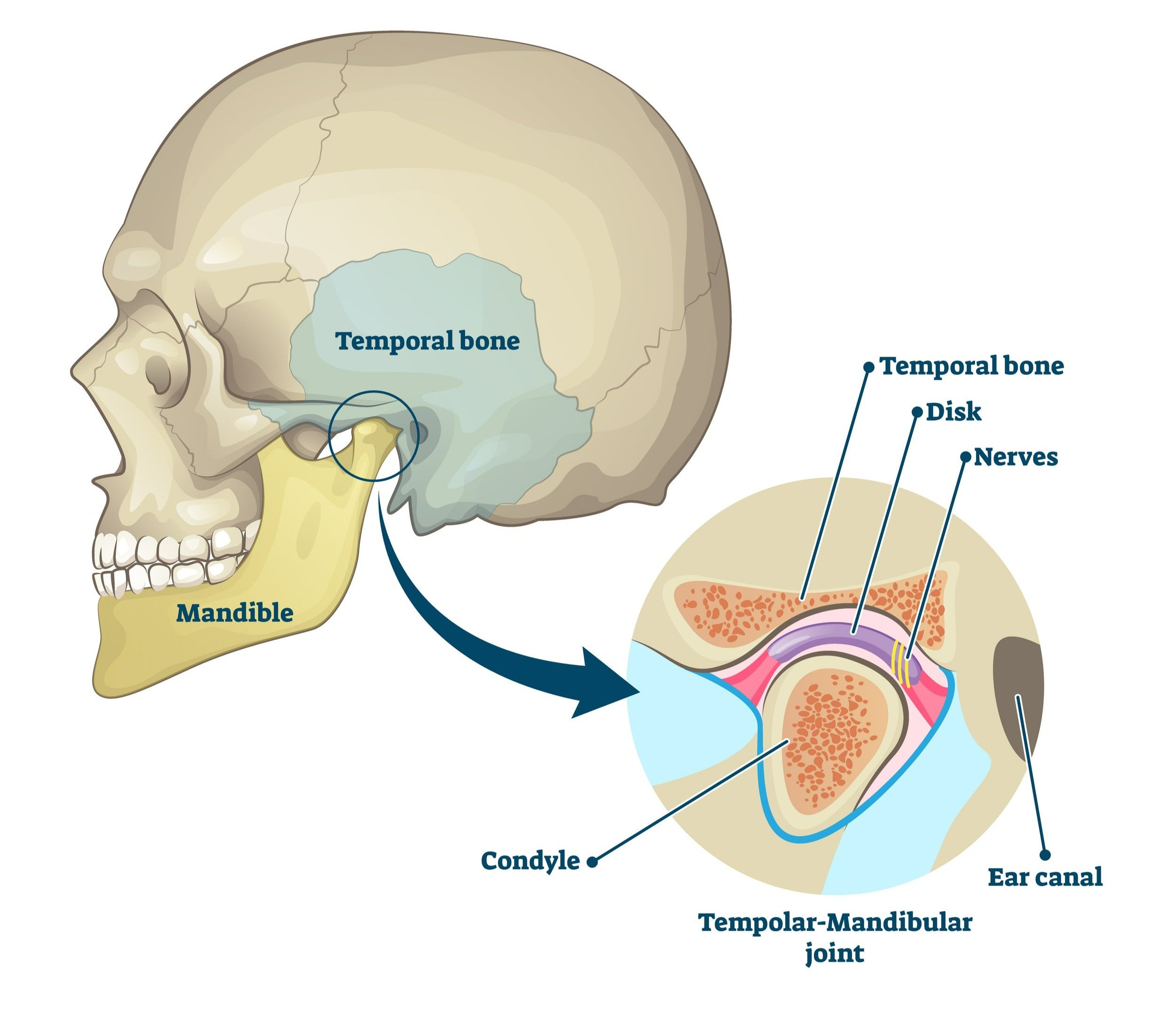
That pesky jaw joint (better known as the temporomandibular joint or TMJ).
So many of us - 35%! - have issues with it yet only 5-10% of us actually seek treatment. Temporomandibular joint dysfunction (TMD for short) tends to hit in people ages 20-40, affecting women more than men.
Despite TMD being so common, not many people know what it is or what to do about it. Here are the top 5 things I want you to understand about the temporomandibular joint and dysfunction:
Top Five Fun Facts About TMJ/D
1. The TMJ moves out of its socket and has a disc
Closed jaw
Open jaw
The TMJ is not your average joint! When you open your mouth fully, the first half of that movement is the jaw rotating in the socket. In the second half, the jaw bone comes out of the joint and moves forward.
The disc is a little piece of tissue that sits on top of the condyle like a hat. It helps the jaw slide nicely out of the socket, holding the jaw in place when the mouth is fully open and returning it to its closed position. Thanks, little disc!
To feel the movement of your jaw, place your hands flat on your cheeks, just in front of your ears. Slowly open your jaw and feel the condyle pop forward into your hand about halfway through opening.
2. Discs can slip forward and that’s okay!
One of the most common causes of TMD is the disc can be displaced anteriorly - in other words, the disc can slip forward in the joint. This may result in clicking or locking of the jaw or it may not - in fact, 9-31% of people moving about their lives have an anteriorly displaced disc and absolutely no symptoms!
The biggest thing to remember with disc displacements is that discs remodel and heal. If you have a symptomatic disc issue, the name of the game is to lessen the irritation of the tissues for a little while to allow the disc to remodel and the TMJ to heal. We do that through manual therapy and specific exercises.
3. Sounds are totally fine, as long as they aren’t painful
Most jaw sounds are related to the discs and if it doesn’t hurt, don’t worry about it. Popping, clicking and snapping are all common sounds in people with no TMJ-related pain.
These sounds are also not predictive of more problems down the road, so ignore them as best you can. It’s hard - the jaw is right beside your ear and the noises can be LOUD! Be armed with the knowledge that these sounds typically decrease over time and everything will be just fine.
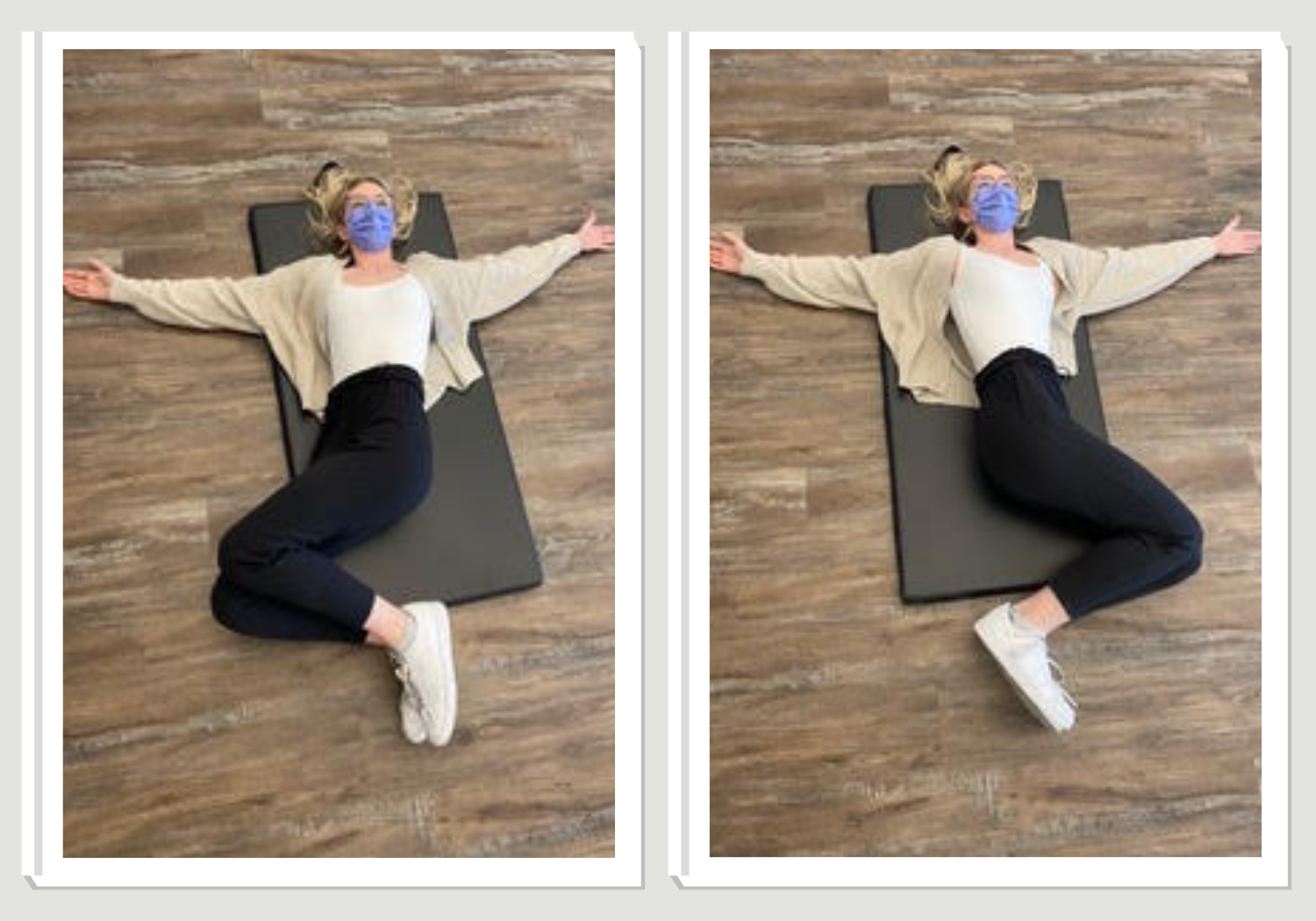
4. Your jaw has a resting position and you should be in it most of the time
Check in with your jaw right now - are your teeth together? Are your jaw muscles clenched, tensed or relaxed? Where is your tongue - is it flopped against your bottom teeth or resting on your palate?
Your jaw should be at rest most of the time. In fact, your teeth should only be in contact for 8-15 minutes per day!
Here’s what you need to look for in a resting jaw:
Teeth slightly apart - your teeth shouldn’t be touching anywhere and be about 1mm apart
Tongue against the roof of your mouth - your tongue should be resting comfortably against your palate. It should be a few millimetres away from your teeth at the front.
Relaxed muscles - the chewing muscles in your cheek and on the sides of your skull should be nice and relaxed.
This resting posture is also heavily dependent on good posture throughout your whole body. For tips on this, visit our previous blog posts on posture Your Head Is A Bowling Ball & Ergonomics: The At Home Edition.
5. All those chewing habits can lead to TMD
We’re talking clenching, nail biting, cheek biting, lip pursing… all those mindless mouth habits so many of us are guilty of doing on a daily basis. All that added muscle activation can lead to overuse of the jaw muscles, causing anything from headaches, pain in and around the face and ear, tooth pain and tinnitus.
Since 45% of TMD is muscular in origin, it’s really important to identify and stop these habits. Changing these habits, like all habits, is really hard to do but it can mean the difference between pain and being pain-free.
If you are dealing with TMD, book with one of our therapists with advanced training in TMD. Book online, through email or call us at (778) 630-8800.