One of the most common jaw complaints is clicking and locking, often associated with pain in the jaw, face, head and down the neck. This can often be caused by an anterior disc displacement, something we see frequently in the clinic.
But what is an anterior disc displacement and what can we do about it? Before we dive into that question, let’s back it up and talk about the anatomy of the temporo-mandibular joint.
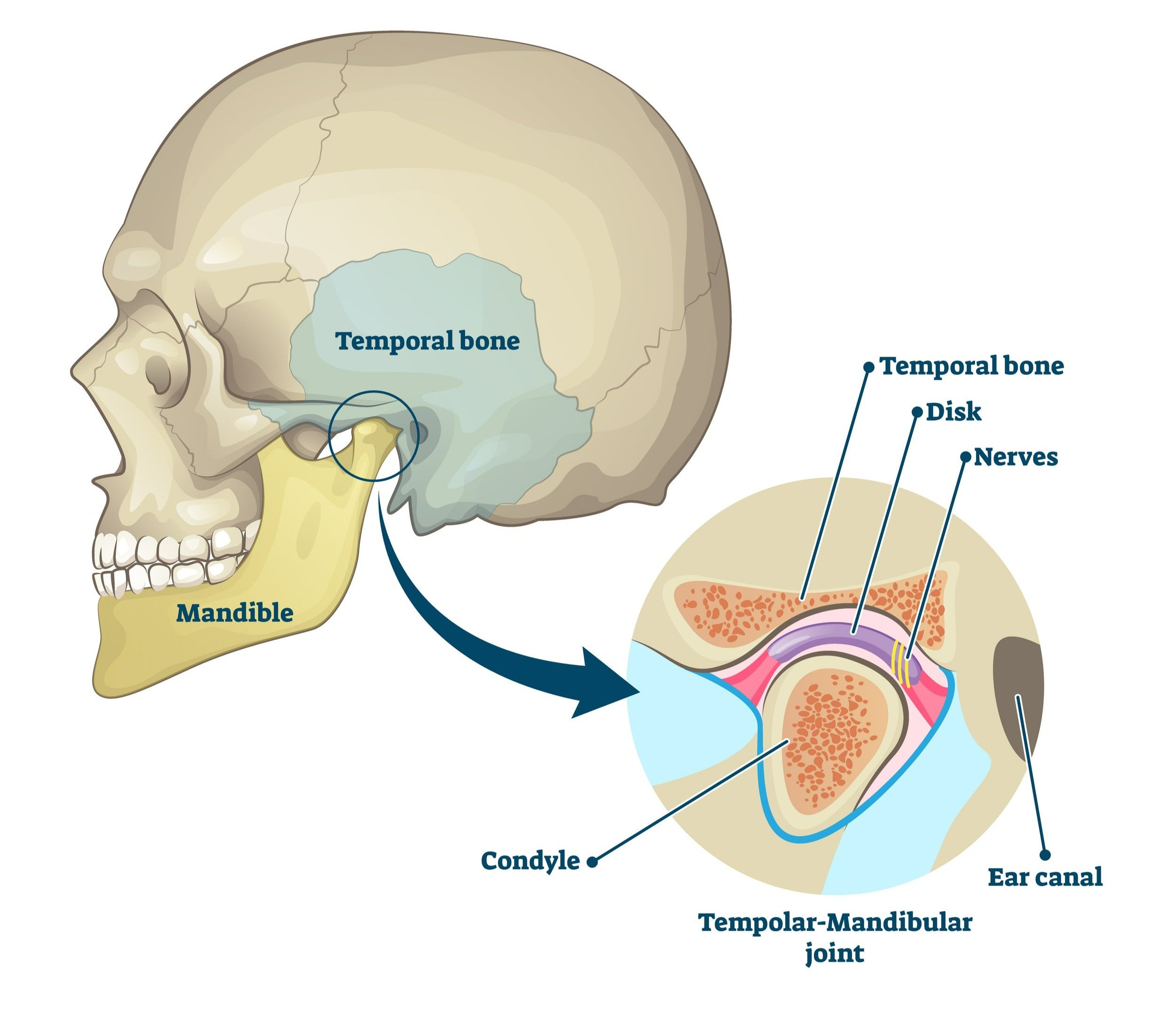
The Anatomy of the TMJ
The temporo-mandibular joint (aka the TMJ) is what attaches the mandible (aka the jaw bone) to the skull. It is located just in front of the ear and, if you place your hands on either side of your face just in front of your ears, you can feel that jaw moving forward and back as you open and close your jaw.
The TMJ is a synovial joint between the temporal bone of the skull and the condyle of the mandible. Between the condyle and the temporal bone is a donut-shaped fibrous disc that is essential for proper opening and closing of the jaw. This disc is partially held in place by the retro-discal tissue, a network of loose connective tissue, blood vessels and nerves attaching the back of the disc to the bone behind it, just in front of the ear canal.
Anterior Disc Displacements
One of the most common causes of temporo-mandibular dysfunction (aka TMD) is when the disc becomes displaced, typically anterior in the joint and away from the ear canal. When this occurs, the retro-discal tissue in the back gets stretched and is unable to hold the disc back in its normal position.
Common symptoms of anterior disc displacements include:
pain in the TMJ with chewing, yawning & talking
pain in and around the ear
headaches
a reproducible click in the TMJ, with or without pain
decreased range of motion with opening
When a disc moves anteriorly in the joint, it may click or block jaw movements but this isn’t guaranteed. Every person’s anatomy is different: jaw condyle shapes, depth of the socket, size of the disc, amount of retro-discal tissue and all the other factors that make a person unique can play into their TMD and experience of pain.
Treating a Disc Displacement
A few things to know first:
One third of asymptomatic people have at least one displaced TMJ disc. It’s really common to have a disc issue and not be bothered by it at all!
Discs will not (typically) relocate back to where they were. Instead, your body heals and creates a “pseudo-disc” from the now-stretched retro-discal tissue to act as the original disc.
When that disc moves forward, it can often block the opening of the TMJ. Over time, the disc remodels to be less donut-shaped and more wedge-shaped so the condyle of the jaw can easily slide over it.
Acute Disc Displacements
Remember how I said just up there that discs won’t relocate?
If the injury has occurred in the past 3 days, we can sometimes (and I stress SOMETIMES) get the disc to relocate. It has to be before the retro-discal tissue has stretched too much. Our therapists who treat TMD can attempt a specific maneuver to try and get that disc back to where it was.
Outside this 72 hour window, we are looking at healing and remodeling the disc.
Chronic Disc Displacements
We have a whole tool-box of therapy techniques to help with disc displacements in the TMJ. These include:
Manual therapy of the TMJ - we use specific techniques to increase the range of motion of the jaw and help the disc remodel into the wedge shape we’re looking for.
Soft tissue techniques (including IMS and massage) of the surrounding muscles - with a disc displacement, these muscles (for instance, the temporalis and masseter) are often clenching or working hard to compensate for the TMD, leading to increased pain and headaches.
Neck assessment & treatment - when the TMJ is irritated, up to 70% of people also have neck pain. As a part of TMD treatment, the neck needs to be evaluated and treated accordingly.
Exercises - the right exercise for you and your TMD is so important. The right exercise helps discs remodel, muscles relax and pain reduce. We spend a lot of time with you to make sure you are doing the correct exercise with the correct technique.
Top Five Tips in Dealing with a Disc Displacement
Finally, we live by these principles of managing disc displacements:
Don’t test it!! You will be tempted - does it still click? Is it still stuck? - but we beg you to resist this temptation. Let your disc heal. The more you poke it, the longer it’ll take to heal.
Avoid hard/crunchy/chewy foods for the first 6-8 weeks after a disc displacement. We promise you can eat your favourite food soon but avoid those types of foods initially.
Support your jaw when yawning. If you have the urge to yawn and really open your jaw, place a hand under your chin so you have something to push against and limit how much your jaw actually opens.
Sleep is so important for healing & pain control. We know that under 6.5 hours of sleep per night increases your experience of pain. We also know that you heal when you sleep. So make sure you’re getting enough sleep, with a good pillow supporting your head!
Posture also play a huge role. Make sure your computer is set up properly so you aren’t sitting in a head forward posture, putting more inappropriate muscular forces through your jaw. (Need some tips on computer set up? Read our blog!)
If you are dealing with a disc displacement, TMD or headaches, book with one of our TMJ therapists online, by email or calling us at (778) 630-8800.