Devon Konrad has been a practicing vestibular physiotherapist for 14 years. In that time, she has worked with many people with vestibular deficits who were given misleading, confusing or just poor advice in how to deal with their symptoms. In this blog, Devon highlights her biggest pet peeves in the world of vestibular rehab.
There’s a certain level of anger I experience when I walk into a new vestibular assessment and I can already feel the client’s walls are up. I then often learn that the person sitting in front of me has been through 1, 2 or more “vestibular therapists” who didn’t help or made things worse. They often come into this appointment with a lot of hesitation and reluctance, expecting the same treatment they’ve had in the past.
Here’s the problem: there is no official accreditation in Canada to call yourself a “Vestibular Therapist”. Anyone can say they are a vestibular therapist, no matter how many (or how few) courses they take or how much mentoring they have received. As a result, Canada is filled with people who highlight “vestibular rehabilitation” as a specialty without actually having the knowledge or expertise to do so.
Balance and Dizziness Canada is trying to change that. They have a list of curated professionals from across the country - physiotherapists, audiologists, occupational therapists - who have taken the gold standard courses in their field. If you are looking for someone who has expertise in vestibular conditions and vestibular rehabilitation, this is a great place to find them.
Until we have a system of accreditation, this will continue to be a problem. So this blog is for all the people out there in the vestibular rehab world, either as patients or practitioners - a What Not To Do, of sorts.
How NOT To Do Vestibular Rehab
1. Keep pushing through symptoms, no matter what
One of my biggest pet peeves is when people have been told they just need to keep pushing and ignore their symptoms; that their symptoms will decrease eventually as long as they just keep pushing.
This. Doesn’t. Work.
Not only does this often put people in a state of perpetual symptoms, it often drives anxiety. And while we don’t have the research yet to implicate poor treatment approaches in developing chronic forms of dizziness, we do know that about about a quarter of people with vestibular deficits go on to develop Persistent Postural-Perceptual Dizziness (PPPD). We also know there is a massive link between anxiety and developing PPPD.
By pushing people into a state of constant symptoms with no locus of control around those symptoms, I argue this is setting people up for longer term problems. Which leads me to my next point…
2. Not learning how to reduce symptoms
When I’m working with someone who has “failed” vestibular rehab, I’ll pick a task that I know will slightly increase their symptoms and then ask them to settle their symptoms.
More often than not, they look at me like I have three heads. Here’s the response I often get: “I don’t know how to settle them! If I knew that, I wouldn’t be here!”
Let me be clear: I’m very good at making people feel dizzy. But my job is to make them feel better and I cannot do that if I’m not teaching them HOW to feel better.
With vestibular rehab, we definitely want to introduce exercises that increase symptoms. You cannot drive the brain changes needed to feel better if you aren’t challenging the brain! But I’d argue it’s even more important for people to learn how to settle these symptoms after increasing them.
Here’s my cues in how to “ground out” and settle symptoms:
I want the person to look at something they are sure is not moving. This could be a light switch, the corner of a table, a lamp shade. Something inoffensive and stable. NOT the curtains, the dog or another human - those things cannot be trusted.
Next, I want the person to really feel their feet. I want them in a wide base of support and paying attention to what their feet are telling them. Some people like to weight shift, some people don’t - it’s whatever feels right for them.
Then, the biggest one - I want slow, deep breaths. The vestibular system and the autonomic system are highly intertwined: when dizziness starts, so does the fight-or-flight response. Breathing cues to the parasympathetic system to bring balance back to the autonomic nervous system, bringing symptoms down.
Finally, I don’t allow people to add more touch points while they recover (unless they’re a falls risk or safety risk - then, by all means, please sit!). If the exercise was done in sitting, they can keep sitting while settling their symptoms. If they were standing, they do not get to lean on a door frame or touch the counter for support. Their brains need to learn how to settle their symptoms without this additional touch point.
I give people about 5 minutes to settle their symptoms in this way. After that, I let them do what they’d like to get their symptoms under control - sit down, lie down, close their eyes, get some fresh air: whatever it is for them.
A good vestibular exercise should stimulate their symptoms enough to be uncomfortable and be able to get back to their pre-stimulated levels of symptoms within 5 minutes. If there’s no symptoms at all, we need to make it harder. If symptoms are taking way longer than this to settle, the exercise is too hard.
Whether they are doing their exercises in the clinic or at home, I drill into them that this “settling piece” is a non-negotiable piece of their rehab. They need to develop a locus of control around their symptoms and have strategies to get those symptoms down. In my opinion, this is the number one goal of vestibular rehab.
3. Not teaching people why things trigger them
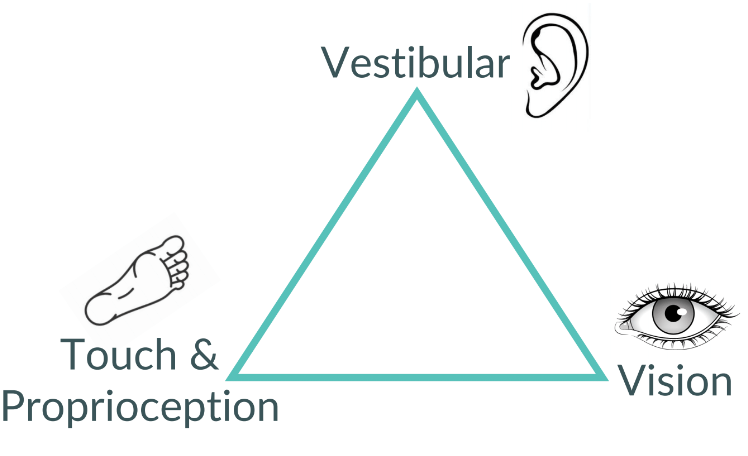
A Triangle of Balance captured in the wild!
In my clinic, you’ll see a lot of triangles written on white boards with “vision”, “vestibular”, and “touch & proprioception” written on them. This is because we spend so much time teaching people about how their vestibular system works as well as how it interacts with their other balance systems. (Want to know more? Check out our other blogs on vestibular rehab!)
Why do we do this? Because people need to understand why they feel the way they do. They need to be able to figure out why their symptoms are up if they’re a passenger in a car, or watching their kid’s soccer game, or skiing in the alpine. By giving them that ability, they can use their strategies to immediately reduce their symptoms and keep them involved in their own lives and doing the things they love to do.
I’m a big believer in making myself obsolete. I want people to leave here filled with knowledge about their vestibular system and how to make their lives work for them. I want them to be able to use their tricks to enjoy the movies on the big screen and play on the playground with their kids.
4. Ignoring symptom burden with exercises and looking exclusively at performance
I see this a lot: instead of asking how people feel during and after their exercises, therapists watch their performance of a specific exercise and make it harder solely on that.
I can see the therapist’s point a bit more in this one - in order to learn new motor patterns, you need to make mistakes so the brain can learn how to correct them. With a perfect performance, you’re not learning much so it makes sense to make the exercise harder.
But what that therapist isn’t taking into account is how awful that exercise is making the person feel. For a lot of these clients, they have just learned how to perform an exercise while feeling awful.
This is not the goal! We are not just trying to make people perform. We are actively trying to strengthen the vestibular system so people feel better. By looking at performance alone, we often miss the most important piece.
This Not To Do list is far from complete but it’s a start! If you’re looking for a good vestibular therapist and don’t know where to start, head to Balance and Dizziness Canada for some great recommendations.
If you’d like to book with us, call us at (778) 630-8800, book online or email us.