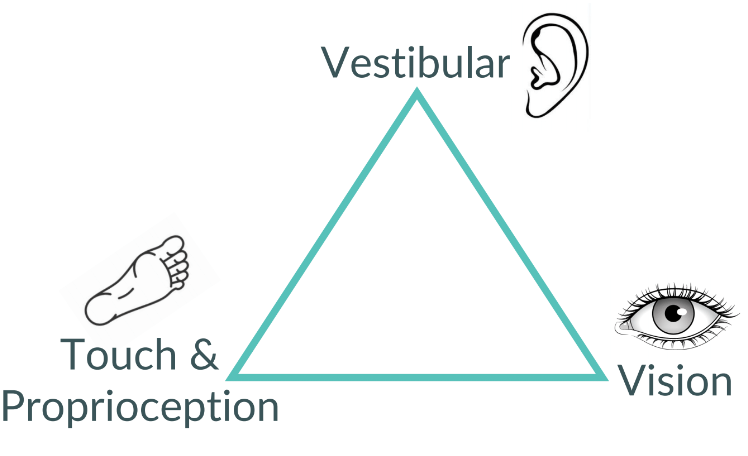
As a vestibular physiotherapist, I talk a lot about the triangle of balance. There are three main inputs to our sense of balance:
Vestibular System - a complex network involving the inner ear, brain stem and cerebellum, the vestibular system is responsible for detecting head movements and the head’s position relative to gravity.
Visual System - another complex network, the visual system goes well beyond the eyes, involving several areas of the brain stem and cerebral cortex.
Touch & Proprioception - these are all the receptors in your muscles, joints and skin telling you what you are touching and where your limbs are in space. If you can touch your nose while your eyes are closed, congratulations! Your proprioception is working!
Vestibular deficits are one of the most common causes of imbalance. BPPV, vestibular neuritis & neuritis, vestibular migraine, and Meniere’s disease are all well-known vestibular causes of imbalance and are all very treatable.
But in reality, balance is a very complex interplay of not only those three things but also cognition, attention, emotion, perception, muscle strength, joint flexibility, pain, motor planning, general stress levels and so much more. Impairments in balance can come from anywhere and have a massive effect on people’s function, especially as we age. With 20-30% of seniors experiencing one or more falls each year and 1 in 5 of those resulting in serious injury, preventing and treating balance issues is imperative.
Other Factors Leading to Imbalance with Age
There are a myriad of factors that can add to imbalance as we age. Here are some of more common ones:
Dehydration - as we age, the part of the brain responsible for telling us we are thirsty becomes less active, leading us to reach for the water bottle less and less. This dehydration can very quickly lead to light-headedness and imbalance.
Medications - several medications list dizziness as a side effect. There’s also a host of medications listing vision changes, light-headedness and drowsiness as side effects, all of which can affect balance.
Walking speed & instability - the slower someone walks, the higher their chance of falls. Combine that with a limp or unsteadiness and imbalance increases significantly.
Foot problems - if people have impaired sensation in their feet, balance problems are likely to follow. Bunions, numbness, thick calluses and ulcerations can directly impact how people are feeling the ground.
Heart issues - a common symptom of cardiovascular disease is dizziness and light headedness especially when untreated.
Vision problems - aging often affects how our eyes adjust to light and distance, taking longer and longer to shift. It’s common for prescriptions to change as we age and people often struggle adjusting to bifocal or progressive lenses.
Cognition changes - so many aspects of cognition affect balance. Multi-tasking takes a lot of brain power and often leads to impaired balance. Cognitive processing and reaction time are critical for maintaining balance. Memory problems are also linked to imbalance.
Fear of falling - one of the leading predictors of imbalance and falls is a fear of falling. People with this fear often do not move nearly as much, leading to inactivity and muscle weakness.
Top Ten Things To Do For Balance (That Aren’t Balance Exercises)
Stay active - the old adage “use it or lose it” is very true, at least when it comes to muscles and the brain. The more active you are, the better. It really doesn’t matter what your passion is, just keep doing it at whatever level you can! Go to the gym or an exercise class to keep your muscles lean, mean and flexible.
Stay hydrated - brains are thirsty and, as we age, our brains forget to tell us. Pay attention to how much water you drink during the day and try to drink at least 8 glasses per day.
Learn something new - your brain never stops changing. It adds new connections and removes connections that aren’t being used. By trying something you’ve never tried before, you are inducing neuroplasticity in your brain. This helps your cognitive power and can help improve balance. The McKee House Seniors Society in Ladner has a whole range of things to try, from line dancing and yoga to water colour painting and ukulele.
Walk with friends - this one checks all the boxes: exercise? Check! Head turns and vision challenges while looking around and looking at your friend? Check! Carrying on a conversation while dodging obstacles? Check! Soul-filling and stress-relieving? Absolutely. Walking with friends should be a part of everyone’s weekly routine.
Cook complex meals or maintain a garden - these are just two examples but the idea is to do complex tasks that take longer than a day to plan for and complete, then require movement to do the task. Other examples are fixing cars, large art projects, being on an organizing committee - the options are endless!
Bring your stress down - stress has a massive effect on your brain. Cognition can become impaired through several mechanisms leading to reduced ability to multi-task, process information and react appropriately. There are several ways to de-stress: yoga, Tai Chi, meditation, boxing, knitting, reading or anything that feels relaxing.
Review your medications with a pharmacist - more than 4 medications is associated with an increased risk of imbalance. Pharmacists are experts in drugs and drug interactions and are the best source of this information.
Be proactive about mental health - anxiety and fear of falling are two of the biggest drivers of imbalance and falls in seniors, with one in five resulting in serious injury. Mental health experts such as clinical counsellors are wonderful resources to address these issues at the root cause.
Have a great relationship with your optometrist - eyes change as we age. Find yourself an optometrist and see them annually.
Treat what needs to be treated - if you’re diabetic, make sure your sugars are in check to avoid peripheral neuropathy. If you have cardiac issues, follow your cardiologist’s advice on medications and exercise. The better you are to your body, the better your balance.
For more on age-related imbalance, head to Balance and Dizziness Canada. You can also find a vestibular therapist in your corner of the world on their practitioner’s list.