The nervous system is incredibly complex. Everything we do, think and feel involves the nervous system at multiple levels. In this blog, we are going to focus on one specific area - the autonomic nervous system: what it is, why it’s important and how we can train it.
What is the autonomic nervous system?
The autonomic nervous system (ANS) plays a pivotal role in regulating vital functions, doing so unconsciously. It serves as the body's autopilot system, controlling involuntary actions such as heart rate, digestion, respiratory rate, and glandular secretion.
It consists of two main branches: the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS), which work together to maintain your body in homeostasis (in other words, to keep everything in balance, from body temperature and heart rate to the amount of oxygen and carbon dioxide in your blood).
1. Sympathetic Nervous System (SNS):
Often referred to as the "fight or flight" system, the SNS mobilizes the body's resources during times of stress or danger.
Functions include increasing heart rate, dilating airways, and redirecting blood flow to vital organs, preparing the body for action.
In rehabilitation, an overactive SNS may contribute to conditions like high blood pressure, anxiety, and muscle tension, requiring interventions to promote relaxation and stress management techniques.
2. Parasympathetic Nervous System (PNS):
Known as the "rest and digest" system, the PNS promotes relaxation, digestion, and energy conservation.
Functions include slowing heart rate, constricting airways, and stimulating digestion, facilitating restorative processes.
In rehabilitation, enhancing PNS activity can aid in promoting recovery, reducing stress, and improving sleep quality, through techniques such as deep breathing exercises, meditation, and progressive muscle relaxation.
(Note - for those of you with an in-depth knowledge of the nervous system, you understand that this is an incredibly simplistic way of talking about the ANS and misses a lot of things, like how poly-vagal theory challenges this framework and the concept of the freeze response. But hey, we all have to start somewhere, right?)
Like anything else in the human body, the ANS can become dysfunctional, leading to wide-ranging effects. Autonomic dysfunction, or dysautonomia, is well documented in spinal cord injuries, Parkinson’s disease, traumatic brain injury and long COVID. There is more and more research looking into stress-induced dysautonomia as a cause for heart disease. Dysautonomia has also been suggested as one of the mechanisms underlying chronic fatigue syndrome and complex regional pain syndrome.
When ANS dysfunction occurs, a multitude of symptoms may result including:
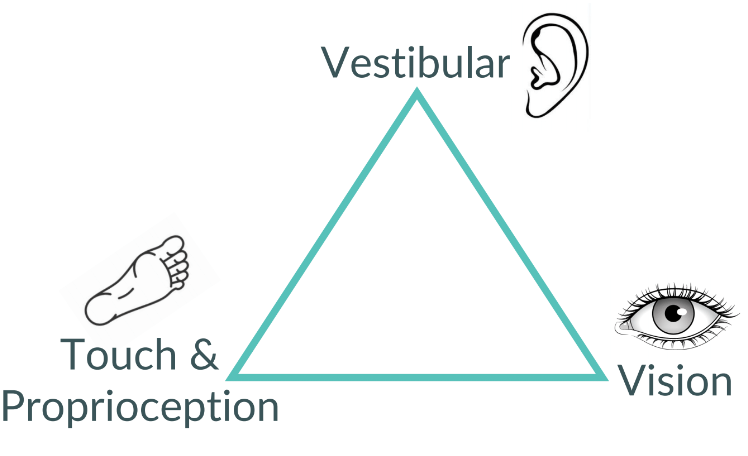
Balance problems
Nausea & vomiting
Brain fog, forgetfulness or trouble focusing
Fatigue
Fast or slow heart rate
Feeling like you cannot regulate your temperature
Sweating more or less than usual
Fainting or passing out
Shortness of breath
Dizziness or lightheadedness
Heart palpitations
Headaches
Exercise intolerance
Mood swings or anxiety
Vision issues
What can I do to help my autonomic nervous system?
While we cannot consciously control much of the ANS, certain practices and interventions can influence its function. Here are some techniques for training the ANS:
1. Breathing Exercises:
Deep breathing exercises, such as diaphragmatic breathing or box breathing, can stimulate the PNS, leading to a relaxation response.
Techniques like coherent breathing, where inhalation and exhalation are paced evenly, can improve heart rate variability and promote ANS balance.
2. Mindfulness Meditation:
Mindfulness practices involve non-judgmental awareness of the present moment, which can help regulate ANS activity by reducing stress and promoting relaxation.
Regular mindfulness meditation has been shown to increase PNS activity, decrease SNS arousal, and enhance overall well-being.
New to mindfulness practice? Try an app like Calm, Headspace or Insight Timer to get started!
3. Physical Activity and Exercise:
Aerobic exercise and physical activity can have profound effects on ANS function, promoting cardiovascular health and improving autonomic balance.
Moderate-intensity exercise, such as walking, swimming, or cycling, can enhance PNS activity while reducing sympathetic arousal.
4. Relaxation Techniques:
Progressive muscle relaxation and guided imagery are relaxation techniques that can help reduce ANS activation and promote relaxation.
These techniques involve systematically tensing and relaxing muscle groups, visualizing calming scenes, or inducing sensations of warmth and heaviness in the body.
5. Yoga and Tai Chi:
Mind-body practices like yoga and tai chi combine physical postures, breathwork, and mindfulness, promoting ANS balance and stress reduction.
These practices have been shown to increase heart rate variability, improve baroreflex sensitivity, and enhance overall resilience to stress.
If you’re looking to add some ANS training into your day, try one! These simple options can help improve sleep, reduce stress and help heal and recover from injury.
Looking for help with your autonomic nervous system, or anything else rehab-related? Book online with us - physiotherapy, massage therapy or kinesiology!