If you’ve seen me around town, I’m usually carrying my bright blue backpack on my shoulders and either zipping around on my bougie cruiser bike (and my new wicker basket!) or walking while zoning out to a podcast. Backpacks are my favourite way to carry my essentials while keeping the weight happily distributed and my hands free.
Like most people I know, I have fallen victim to poor backpack habits in the past. I have definitely been that person in class treating my pack like a clown car, pulling out item after item and desperately trying to find the thing I need. At the end of those days, it was all I could do to pop an Advil and get in the bath - not exactly the smartest thing to do.
So, dear reader, it’s a great time to learn from my mistakes! Let’s go over the essentials of backpack wearing - how much weight is appropriate, how to pack your backpack and what red flags you should pay attention to.
Top Ten Backpack Wearing Tips for Back To School:
Ensure your pack weighs no more than 10% of your body weight. We commonly hear that 15% is the upper limit, but current research questions this number. Another journal article identifies “significant biomechanical, physiological and discomfort impacts on the wearer, especially with loads above 10% of the student’s body weight”. The take home? Keep it under 10%.
Buying a new pack? Go for wide straps and a padded backing. The cushion will help distribute the weight and make it much more comfortable especially on long days.
While you’re at it, make sure the pack actually fits your back. Try it on (preferably with some weight) - the bottom of the back should be right around hip height and not hitting your bum.
Use both straps. Please, for the love of everything holy, distribute that load across both your shoulders.
If your pack is particularly heavy one day, use the waist strap. It will help keep the load closer to your centre of gravity and distribute some of the weight from your shoulders to your pelvis.
Place heavy things close to your body at the back of the pack. There’s a reason the laptop pouch is at the back of the bag (beyond the whole projecting the valuable thing part) - it keeps the weight close to your body’s centre of gravity and places less stress on your muscles and joints.
Use those multiple compartments. They keep your load spread out and in place, reducing the chance of injury from load shifting.
Putting your backpack on and off should be easy. If you’re struggling, it means your pack is too heavy.
If you’re leaning forward to carry your pack, it’s too heavy. Your backpack shouldn’t be pulling you backwards. If it is, back pain won’t be far behind.
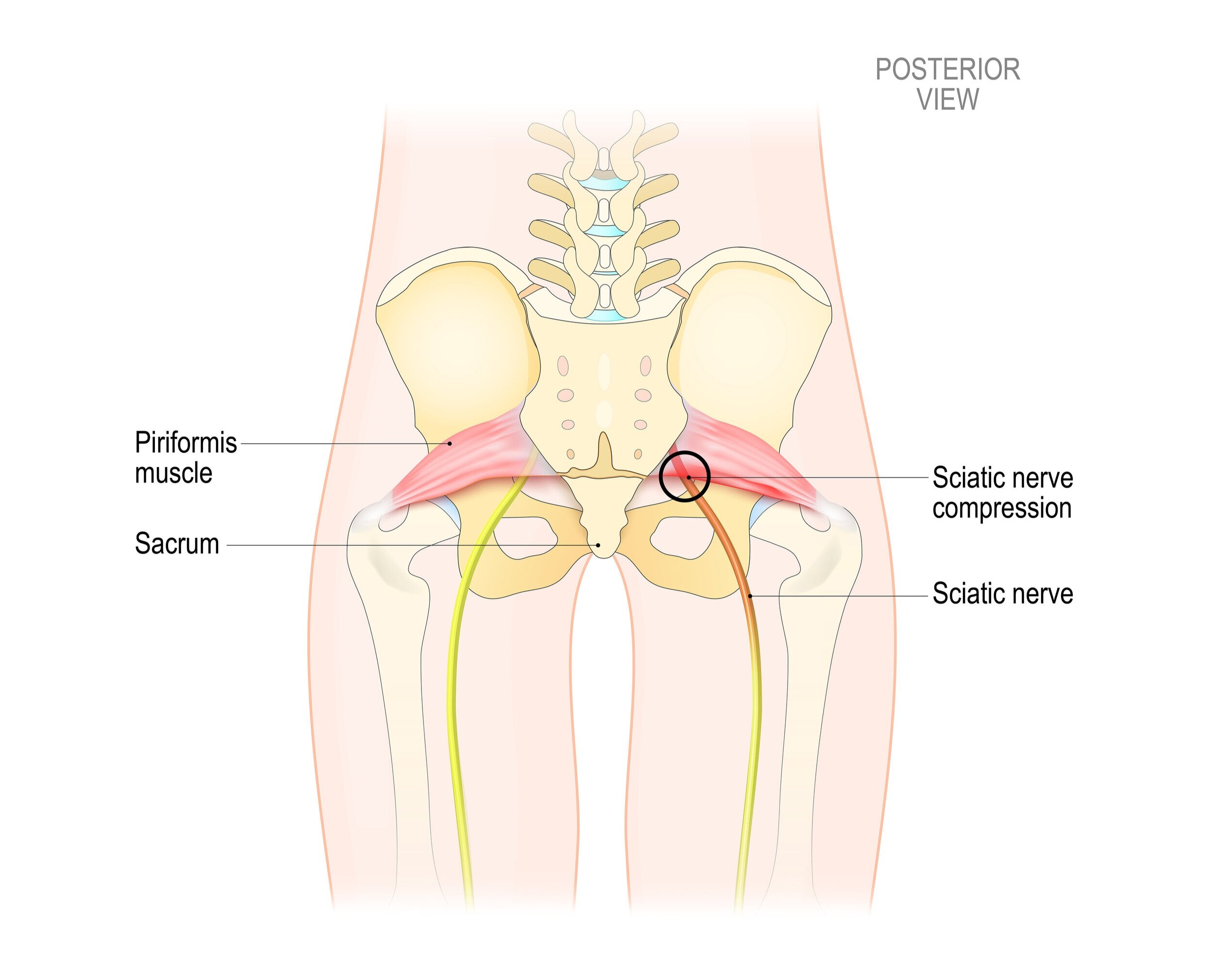
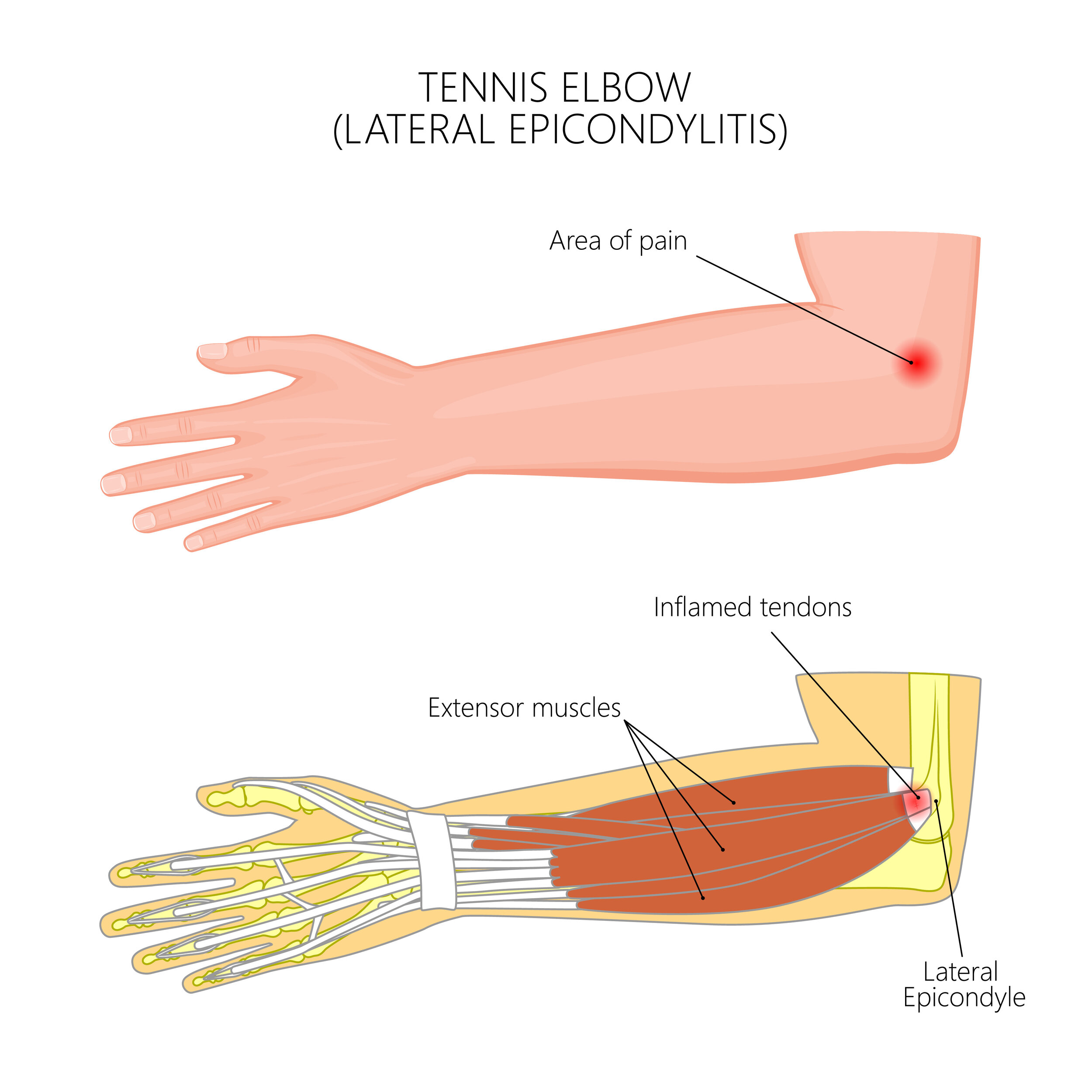
Other signs of too much weight in your pack: neck pain, tingling and/or numbness in your shoulders, arms or hands, and visible strap marks show up on your shoulders. If you start experiencing any of these signs, it’s time to re-evaluate your pack situation ASAP.
We see a lot of poor backpack practices lead to postural changes and pain. Develop good habits early and avoid the problems down the road - you’ll be happy you did!
If you’re suffering with backpack-related pain, give us a shout at (778) 630-8800, email us or book online.