Whenever I am doing an initial intake interview with a client who has come in with concerns about their pelvic floor I ask about prolapse. The most common answer I get when asking if people have any concerns about prolapse is simply “what the heck is prolapse?” Well, let me tell you.
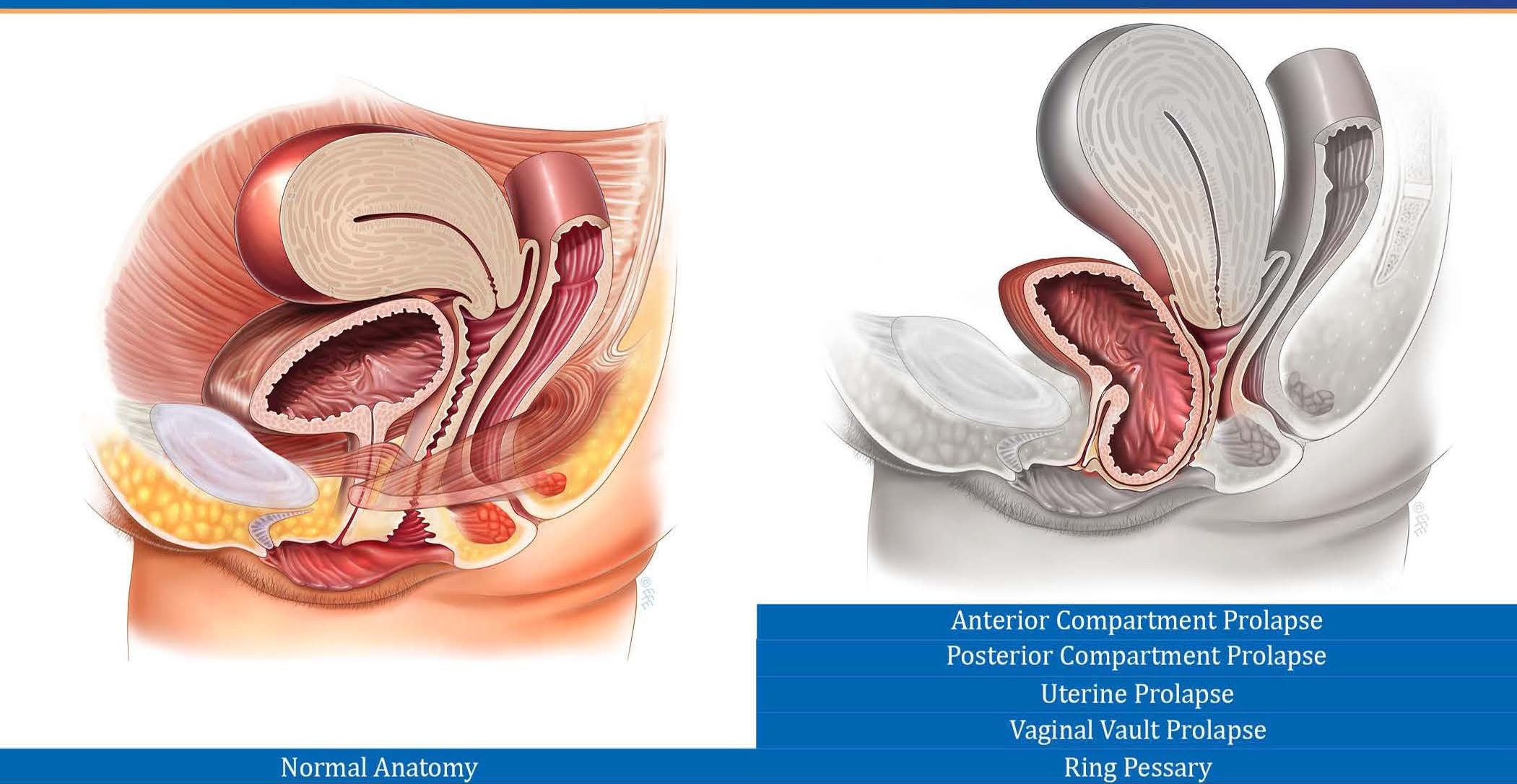
You have various organs within your abdominal cavity, the lowest of which include your bladder, your uterus and your rectum. They are all strapped into place and held in the correct position with connective tissue, like a marionette being held upright by strings. But sometimes those strings get over-stretched (like during childbirth). So instead of having nice upright puppets you now have puppets with extra long strings, which means you now have droopy puppets. These “droopy” organs then begin to collapse downwards.
It’s like your vagina is a tent (yes, like a camping tent), and then a big old bear (aka one of your organs such as your bladder) comes and sits on the edge of your tent. The bear is not physically inside your tent, but he’s leaning on it and squishing it, and making the space inside your tent smaller. This can lead to a “bagginess” or “sagging” within the vaginal canal which is also known as prolapse!
Women who have a prolapse (that they are aware of) generally describe sensations of vaginal heaviness, pressure, of something being inside of their vagina (like a tampon or a “bubble”), or a general feeling of their “insides falling out.” This can occur all day every day or occasionally. Often activities such as coughing, sneezing, carrying something heavy, or being on your feet all day can increase awareness and sensations of the prolapse. That being said, many women have a prolapse and have no sensation of it at all. This applies to small, moderate, and large prolapses. Some women have tissue protruding outside of their vagina for the majority of the day but if you asked them to stand clothes-free and hands-free they would have no awareness that their anatomy was different or changed.
The name of the prolapse will depend on the structure causing the issue. I have listed a few of the more common terms below:
Anterocele/cystocele/anterior vaginal wall prolapse: these are all generally names used for when the bladder is the offender. When the bladder decides to droop, it collapses into the empty space of your vaginal canal. This can sometimes lead to symptoms such as incomplete bladder emptying.
A rectocele is also known as a posterior vaginal wall prolapse. This is when the back wall of your vagina (the wall between your vagina and rectum) is pushed forward due to external pressure from the rectum. Please note that a rectocele is not the same as a rectal prolapse. This is when tissue is loose inside the rectum resulting in excess tissue bulging out of the anus. A rectocele can cause, among other things, difficulty initiating a bowel movement.
A uterine prolapse is pretty straight forward. If your uterus is dropping it’s more like the tent is collapsing from above. It can sometimes “drag” the front and back walls of the vagina down with it and seems to be the most noticeable type of prolapse.
You can usually tell which structure has prolapsed with a brief self exam. If you put your finger inside of your vagina and it feels squishy in the front, it’s a cystocele. Squishy in the back is a rectocele. If the extra tissue feels firm like the end of your nose you are feeling your cervix and it means that your uterus is the structure that has dropped.
The grade of a prolapse will depend on how much “droop” there is. If the bagginess is happening in the upper half of the vaginal canal it’s a grade 1. If the bagginess is in the lower half of the vaginal canal it’s a grade 2. If there is tissue protruding out the entrance of the vagina the prolapse is a grade 3.
Treatment options for prolapse vary and the right option for you will depend on a few things such as A)which structure is prolapsed? B) how big is the prolapse? And C) how much does it bother you?
I will discuss treatment options for prolapse in my next blog, but if you have any specific questions or would like a consultation please feel free to contact the clinic or book an appointment and I would be more than happy to help you out!
If you’re looking for the second half of this blog, check out Part 2 - I Have A Prolapse! Now What?