Nicole Coffey is our resident pelvic health guru and expert on all things related. Read as Nicole answers a Q& A about what exactly a pessary is and who could benefit from one.
What is a pessary? I get this question a lot.
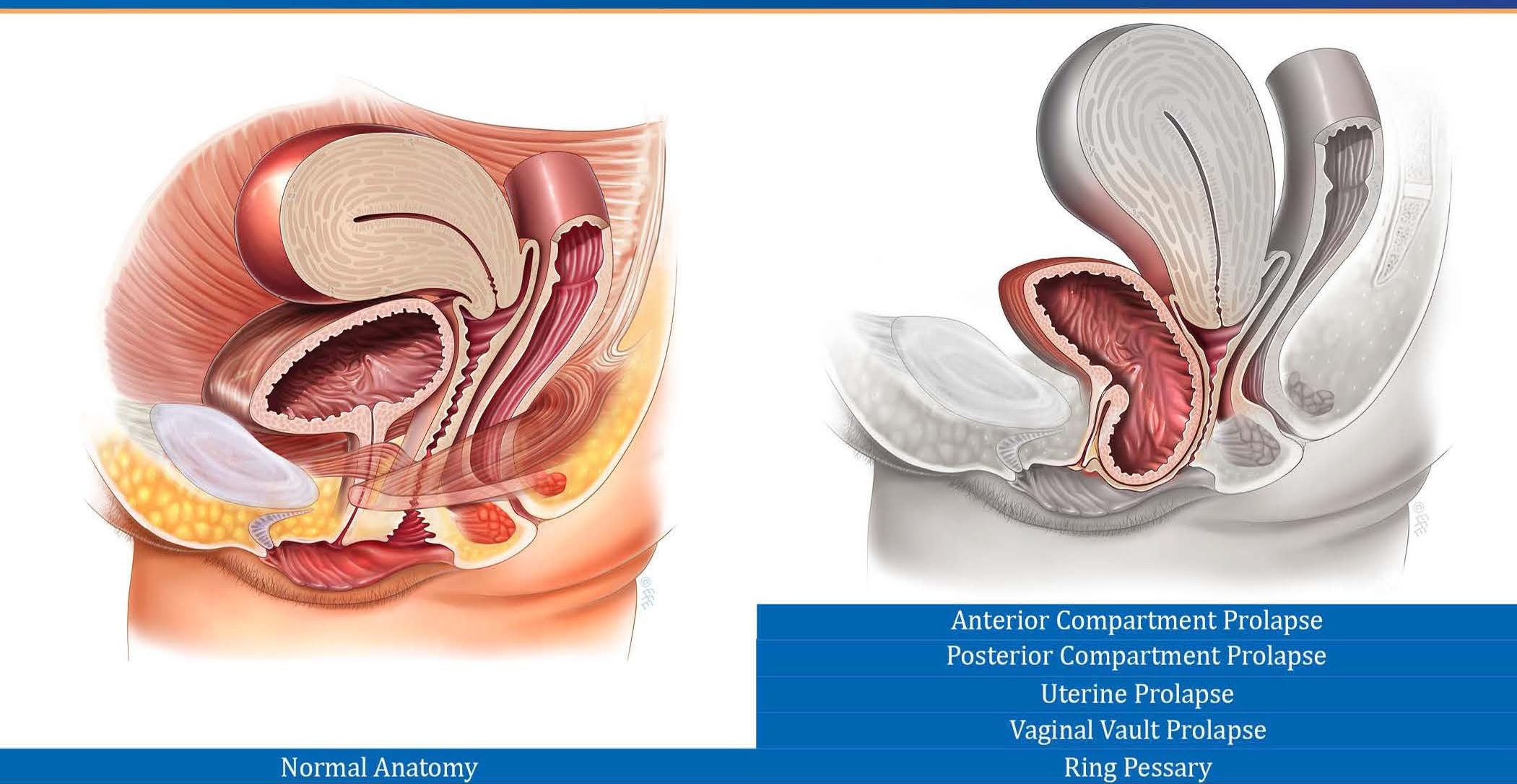
A pessary is an internal vaginal support device typically made of medical grade silicone. They are generally used by women who experience bothersome symptoms from prolapse (when one or more of the abdominal organs including the bladder, uterus or rectum descend and decrease the space within the vaginal canal - find more information in my earlier blogs Part 1: What is Prolapse? and Part 2: I Have A Prolapse! Now What?). This can lead to symptoms such as vaginal heaviness, pressure, a sensation that something is “up there”, or noticing tissue protruding from your body. There might also be bladder and bowel symptoms such as incomplete emptying. Pessaries can also be used to treat urinary stress incontinence, which is accidental urine leakage with activities such as coughing, sneezing, jumping, running, and so on. The pessary acts like an internal shelf to hold the organs up, keeping them away from the entrance of the vagina.
Typical Pelvic Floor Anatomy
Uterine Prolapse
Inserted Pessary
For some people, surgery is an option. For people who do not want to have surgery or who are not surgical candidates, a pessary can be a fantastic option for treatment. (For the record, pelvic floor exercises are also awesome and can help as well, but we are talking about pessaries today).
So what holds people back? Pessaries can be intimidating. But have no fear, I am here to show you that they aren’t so bad after all!
Take a look at the most common questions I get about pessaries:
1. Do they hurt?
No! The best thing about a pessary is when it is inserted you can’t feel the pessary and you can’t feel your prolapse! This is why they are so magical. Some women who have a history of vaginal pain (such as pain with intercourse and tampon use) might have discomfort while inserting and removing the pessary. Other women report an initial discomfort when inserting and removing the pessary until they get the hang of it but the majority of users report no pain. If you do feel pain when inserting and removing the pessary and you are post-menopausal you might benefit from vaginal estrogen cream (this is an excellent conversation to have with your doctor).
2. Are they hard to get in and out?
Not really. Some styles are trickier than others and require a little bit of skill, but with a little bit of practice you will be a pro at managing your pessary.
3. When do I wear it?
This is mostly up to you. Some women only wear their pessaries during high intensity exercise. Some women insert it every morning and remove it every night. Others wear theirs for 3-5 days at a time. If a gynaecologist fits you with a pessary there is an option to wear it for longer periods (up to 3 months at a time), but this again is a conversation to have with your specialist.
4. Can I have intercourse when I am wearing my pessary?
Usually no. There are some types (ring pessaries) that would allow for penetrative vaginal intercourse, but the majority of pessaries need to be removed for intercourse.
5. How soon after having my baby can I be fit with a pessary?
I personally do not fit people with pessaries before 12 weeks post-partum because your body is still healing and changing. I also do not fit people who are currently pregnant. Again, if you see a gynaecologist they will be able to work with you in these situations as needed.
6. I don’t have prolapse but I leak urine, can I still use a pessary?
If you leak urine due to stress incontinence (coughing, running, jumping, etc.), a pessary absolutely can help. It will probably just be a slightly different type and you likely will only have to wear it at times that you leak such as while at the gym. A pessary will not help with urge incontinence (leaking due to a very sudden and strong urge to pee).
7. How do I know what size and type I need?
This one is unfortunately a little tricky. Fitting a pessary is a combination of experience, art, and some trial and error. During your appointment I discuss with you which type of pessary I think would be best for you to try first and why. Then we proceed to try a few different sizes and shapes as needed until the perfect one is found. Sometimes this happens right away and sometimes it takes a few tries. It might take more than one appointment but it is worth it in the end to have a pessary that fits properly.
If you have any further questions about pessaries or would like to book a pessary fitting, book online, send us an email at clinic@ladnervillagephysio.com or give us a call at (778) 630-8800.