OK, so you have prolapse. What do you do about it?
Treatment for prolapse depends on a few different factors including (but not limited to):
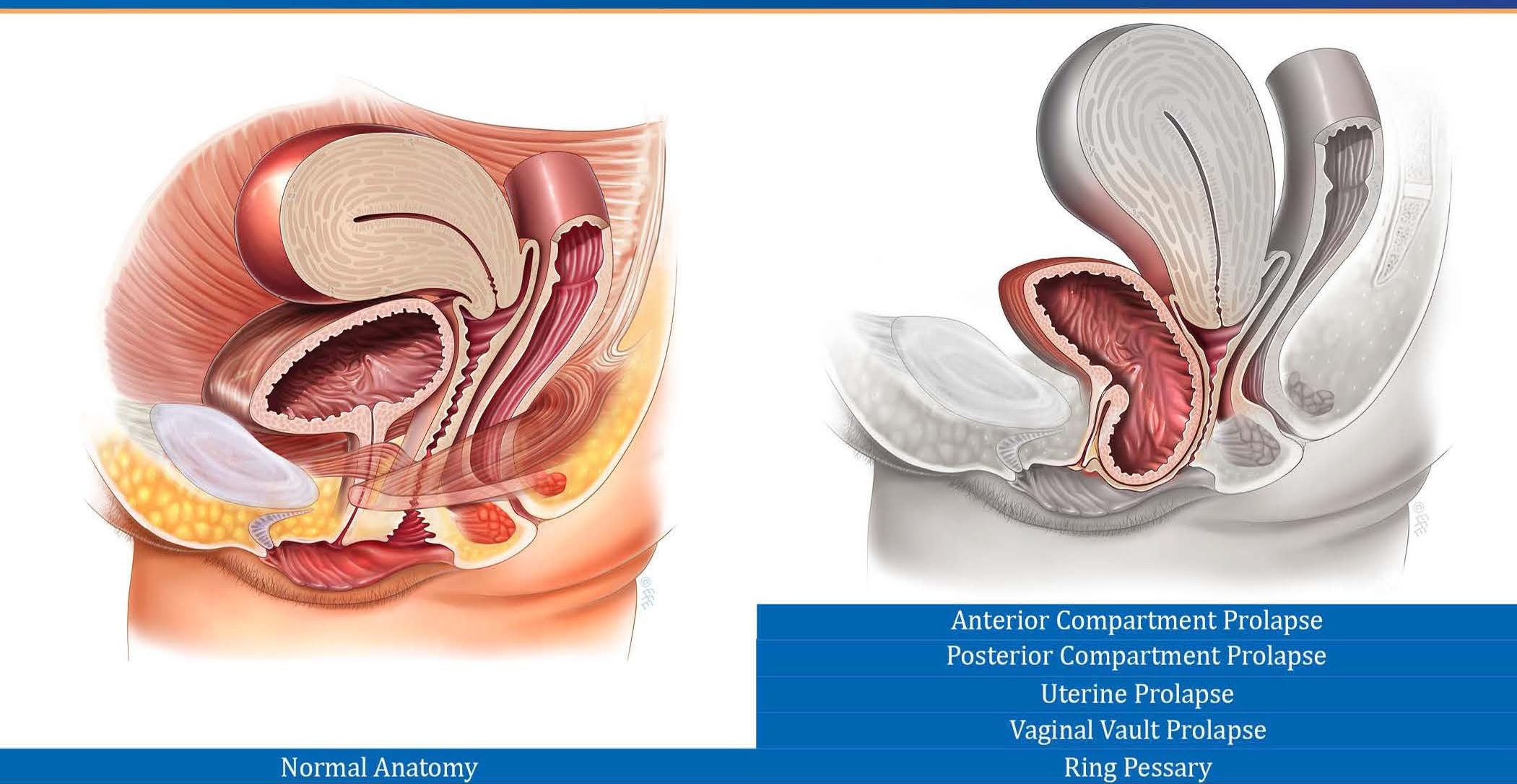
Which structure(s) is/are prolapsed? (Anterior wall, posterior wall, uterus?)
What is the extent (grade) of the prolapse? (I covered the grading in my previous blog, but for a brief refresher Grade 1 = mild, Grade 2= moderate, grade 3 = large).
How much is it bothering you? (Depending on the type of prolapse some things you might notice include sensations of vaginal heaviness or pressure, incomplete bladder emptying or trouble initiating a bowel movement).
A pelvic floor physiotherapist can help guide you as to which exercises and precautions are most appropriate for you and your specific situation.
The three primary treatment options for vaginal prolapse are:
Pessaries
Pelvic Floor Exercises. Pelvic floor exercises are fantastic because they are easy to do, inexpensive, non-invasive, and fairly effective. I often say that running with prolapse might feel a bit like running without a bra on (not my favourite feeling in the world). But with a little strength and skill your pelvic floor musculature can become the sports bra. It can be strong and work to support the prolapse throughout the day, maybe even provide a little bit of lift. While pelvic floor exercises are useful and helpful, they are not a quick fix, nor are they magical. They are often more than enough for women with only minor bother symptoms or mild/moderate prolapse, but they cannot turn a prolapse that is protruding outside of your body (grade 3) into a “barely there” grade 1.
A Pessary. If pelvic floor muscles are the sports bra then a pessary is a sports bra with underwire! If you have never heard of a pessary you aren’t alone. Essentially, they are silicone vaginal support inserts (maybe like an ankle brace, only for your vagina) that work to lift and support the prolapse. I get that this sounds intimidating, but here is the thing…. When a pessary is inserted (and fits correctly) you can’t feel the pessary and you can’t feel the prolapse! You read that right. It essentially takes your prolapse bother symptoms away (whatever they might be, such as feelings of vaginal heaviness, pressure, etc). Pessaries come in many shapes and sizes and have different wearing patterns. Some women only wear a pessary while exercising. Others insert it every day and take it out every night. Some people wear the pessary for several days at a time. There is some upkeep involved such as cleaning the pessary and follow up visits to ensure the pessary fits correctly. They are a successful long-term management tool as an alternative to surgery.
Surgery. This is the only “true fix” that is not just supporting from below but actually “re-stringing” from above. It is also obviously the most invasive procedure. Each gynecologist and surgeon will have their own protocols so I suggest having an in-depth conversation with your specialist if you are considering the surgical route. Surgical recovery times and potential complications such as re-occurrence rates are all important questions to ask.
One big consideration, no matter which treatment route you choose, are steps you can take to help prevent further progression of the prolapse. These can include avoiding chronic constipation, minimizing high impact activity, being mindful of correct lifting techniques to name. Or maybe you have no sensations of vaginal heaviness but do experience symptoms such as incomplete bladder emptying or trouble initiating a bowel movement. These could also be a sign of prolapse.
If you have any questions about prolapse or would like to book an assessment please feel free to email us at clinic@ladnervillagephysio.com or phone the clinic at 778-630-8800.
Wondering where to find Part 1? Right here - Part 1: What is Prolapse?


















![IMG_9593[17310].jpg](https://images.squarespace-cdn.com/content/v1/5b934a448ab722e183624e30/1551243769420-HXZ428J6L39EFPLQTKBB/IMG_9593%5B17310%5D.jpg)
